Kidney Removal: Description, intention, and variations
A living donor undergoing nephrectomy is a selfless act that can save someone's life. Before the operation, the donor typically meets with their treatment team, which includes a surgeon, anesthetist, nurse, healthcare assistant, specialist cancer nurse, dietitian, and physiotherapist.
The primary reason for a living donor to undergo nephrectomy is to donate a kidney to someone with kidney failure. To ensure the donor's safety and compatibility with the recipient, a rigorous evaluation and testing process is carried out.
The Evaluation Process
This process includes blood group compatibility tests to match donor and recipient blood types, a physical examination and assessment by a transplant doctor, various laboratory tests, imaging studies, screening for infectious diseases, and evaluations to ensure donation will not compromise the donor's health and well-being.
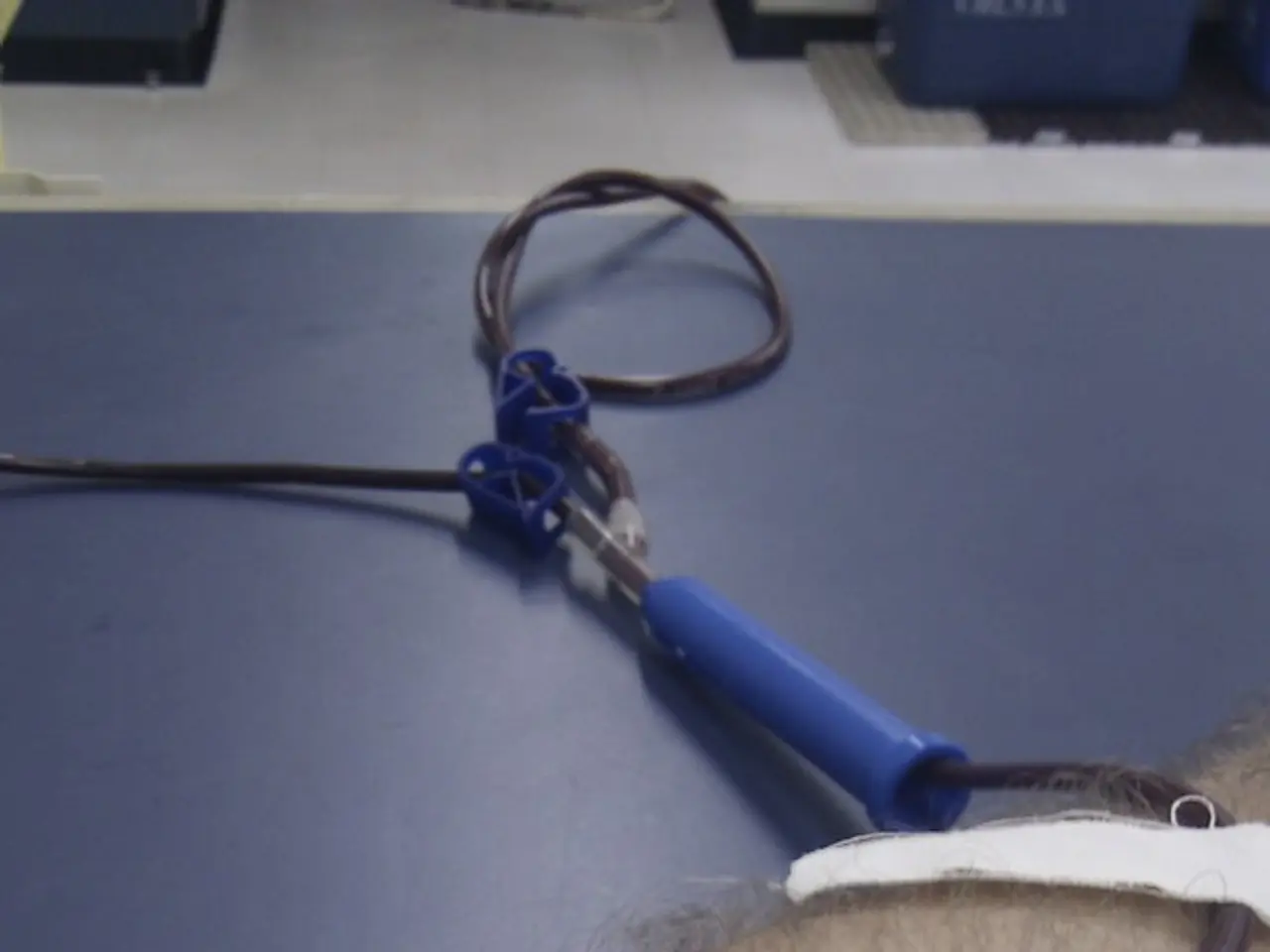
Blood tests and urine tests are conducted to check kidney function, while imaging studies such as chest X-rays, electrocardiography (ECG), CT scans or MRIs, and renal arteriography (if needed) help visualize the kidneys and vascular anatomy. The screening process typically takes at least two weeks, balancing donor safety and transplant success.
The Nephrectomy Procedure
The nephrectomy itself is often performed laparoscopically through small incisions for faster recovery. There are two main types of nephrectomy: partial, where only part of the kidney is removed, and radical, where the entire kidney is taken out. In robot-assisted nephrectomy, a robotic system like the da Vinci Surgical Robotic System allows the surgeon to perform the surgery remotely with greater precision.
Open nephrectomy, which requires a single wider incision in the abdomen and often removal of a rib, is more invasive. Laparoscopy, a minimally invasive procedure involving three to five small incisions on the abdomen and a camera to visualize the kidney, is an alternative option.
Risks and Recovery
Nephrectomy carries potential risks such as bleeding, infection, puncture of the lung cavity, post-operative pneumonia, kidney failure, abdominal wall hernia, urine infection, cardiovascular problems, allergic reactions to anesthesia, and fatal outcomes in rare cases. However, a donor can live a long and healthy life without complications after donating a kidney.
Both the donor and recipient can live a healthy life with one functioning kidney. Nephrectomy is one of the main treatment options available for kidney cancer and is often successful if the disease has not spread beyond the kidney. The nephrectomy may also be necessary to treat kidney damage, kidney stones, kidney trauma, shrunken kidneys, or other reasons.
In summary, living kidney donation is a life-saving act that involves a rigorous evaluation and testing process to ensure donor and recipient compatibility and safety. The surgery itself is often performed laparoscopically for faster recovery, and both the donor and recipient can lead healthy lives post-surgery.
The rigorous evaluation process for living kidney donation includes blood group compatibility tests, physical examinations, various laboratory tests, imaging studies, screening for infectious diseases, and assessments to ensure the donor's health and wellness are not compromised.
The nephrectomy procedure could involve a laparoscopic, robotic, partial, or radical approach, with laparoscopy being a minimally invasive option.
Nephrectomy carries risks such as bleeding, infection, and kidney failure, but donors can live long and healthy lives without complications after the procedure.
Living kidney donation can save someone's life, and both the donor and recipient can lead healthy lives with one functioning kidney, making it an essential treatment option for various medical conditions, including kidney cancer and kidney damage.