Medicaid Eligibility Changes: A Look at the Implications for Beneficiaries due to Fresh Regulations
In a significant shift, certain Medicaid recipients are now expected to comply with work requirements, volunteer activities, or job training programmes, clocking in at least 80 hours per month. This new policy, which has already been implemented in some states such as Georgia, Arkansas, Idaho, and South Dakota, is still awaiting final approval in Missouri and Oklahoma.
However, the implementation of these work requirements has sparked controversy. Some advocacy groups argue that these policies disproportionately impact vulnerable populations and could potentially violate federal Medicaid law. As a result, legal challenges are expected to continue throughout 2025, with federal courts reviewing the legality of these requirements.
It's important to note that exemptions do apply to certain groups, including seniors over the age of 65, pregnant women, people with documented disabilities, and primary caregivers of young children or disabled family members. Some recipients may also automatically qualify for exemptions.
Recipients are advised to keep records of their hours worked, job search activities, or volunteer service to report accurately each month. They should also create an online account with their state Medicaid agency to track work and reporting requirements. Missing reporting deadlines could lead to disruptions in coverage, even for eligible individuals.
For official updates, visit your state's Medicaid website or contact your caseworker directly. It's crucial to stay alert for updates from your state and national agencies like the Centers for Medicare & Medicaid Services (CMS).
The future of these work requirements remains uncertain. Depending on court rulings later in 2025, some Medicaid programs may be delayed, paused, or overturned. It's essential for recipients to stay informed and comply with the requirements to avoid temporary suspensions or loss of coverage.
Remember, staying informed is key. Sign up for FingerLakes1.com's Morning Edition to receive the latest headlines each morning, and keep abreast of the latest developments in Medicaid work requirements.
Read also:
- Guide to Effective Utilization: Advanced Practice Providers - A Comprehensive Video Tutorial
- Conventional Medicine's Domain Shrinks as Complementary and Alternative Therapies Gain Popularity
- Restoring SCN2A gene function in mice through CRISPR activation enhances neurodevelopmental outcomes.
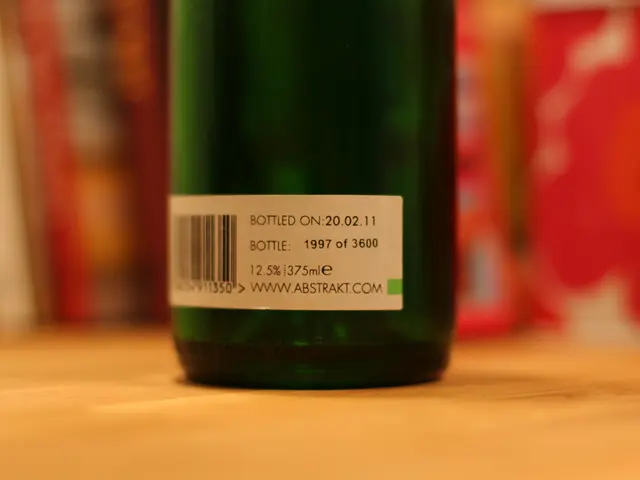
- Tracking Grapes for International Shipping